A patient with vestibular schwannoma required intraoperative neuromonitoring (here). Symptoms were one year of right hearing loss, right face numbness, numbness in the inner right oral cavity until the pharynx. Motor movements are normal for all cranial nerves (6th, 7th, 11th, 12th).
PREOPERATIVE STUDY
Facial nerve motor neurography (with simultaneous recording from Orbicularis oculi, Orbicularis oris and nasalis muscles showed reduced CMAP amplitude with preserved velocities in the right side all investigated muscles.
Blink reflex (supraorbital nerve - V to Orbicularis oculi - VII) showed delayed R1 in the right side with conserved R2 morphology in both sides when stimulation was applied to the right side and normal R1 with reduced amplitude of R2 components when stimulation was applied to the left side.
There were signs of mild facial nerve neuropathy (“axonal” or neurapraxia) in the right side.Blink reflex showed abnormal afferent component (5th) in the right side.There are objective findings of 5th and 7th nerves involvement. The IONM protocol will include corticogeniculate MEP (Co-MEP), SSEP, mapping of cranial nerves and trigemino-facial monosynaptic reflex (R1).
|
INTRAOPERTIVE NEUROMONITORING
Procedure and Results |
Before
the anaesthesia nine “10-20” scalp locations were marked (Fpz, Cz, Cz’, C3, C4,
C1, C2, C3´and C4´). In the operating room and previous to neuronavigation and
fixation moment, in dorsal decubitus position, with total anesthesia and
orotraqueal intubation, we introduced hook wires electrodes in both palatoglossus
muscles, both orbicularis oculi, both orbicularis oris, both masseter, right
nasalis, right mentalis, both hypoglossus, both APB, left AH and left TA
muscles.
Modalities:
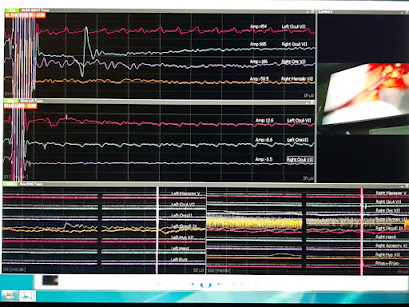
Spontaneous EMG, transcortical MEP, corticogeniculate MEP (Co-MEP), SSEP, blink
reflex, monopolar and bipolar cranial nerves mapping (trigeminal –masster, facialis
–orbicularis oculi, nasalis, orbicularis oris, mentalis, vagus –palatoglossus, hypoglossus
–tongue).
MEP: “train of five” technique from C2-C1
SSEP: from tibialis nerve and median nerve, recordings from Cz´-Fpz and C4´-Cz’ channels
Co-MEP:
were obtained from orbicularis oris and mentalis in the right side, from
C3-Cz and C4-Cz
Blink
reflex: was useful during the entire procedure. We used a train of 6 pulses
(right side) and 3 pulses (left side) with 149uS duration and a frequency of
0.5Hz (rabndomness of 10-20%). Intensity was 102 V in the right supraorbital
nerve and 50 V in the left supraorbital nerve.
Scalp
EEG from cork screw electrodes: 6 channels.
BAEP
At
the end of the surgery we performed zygomatic nerve – palatoglossus
(V-X) reflex.
Results:
MEP,
SSEP and CoMEP modalities showed similar signals at the end of the surgery.
Mapping
techniques were useful to localization of the hypoglossus, vagus and facialis
cranial nerves with thresholds low up to 3-5mA for monopolar stimulation (not
more than 12 mA) and 0,29-0,43mA for bipolar facialis mapping.
Raw
EMG:
Incidence:
In two occasions we observed spontaneous discharges of “A train” first time in mentalis muscle (less than 15 seconds
duration) and the second time in bursts of less than 2 seconds (during less
than 10-15 seconds) in orbicularis oris
muscle. “B train” was seen in one occasion during less than 10 seconds. These
discharges were rapidly communicated and we assumed they corresponded to
manipulation or “debulking” near the facial nerve.
Blink
reflex: showed delayed latency in the right side, but it was the modality used
during the entire surgery and it show good responses even during spontaneous
neuromyotonic changes assuming that the nerves were intact.
Trigemino-vagal
reflex: at the end of the surgery a new modality was set in a protocol to
assess the palatoglossal status. The reflex was observed with a latency of more
than 20 ms in both palatoglossal muscles (in the picture the name of the
channel is LGF and RGF) but no record was seen from hypoglossus muscles
(tongue) or masseter muscle.
Conclusion:
The
tumor was removed in proportion of 50-60%. We assumed that there would be no
long-lasting new neurological deficits in the analyzed and monitored cranial
nerves.
The
patient had postoperative diplopia, followed the examinator finger to both
sides, facial and hypoglossal nerves looked to be with no new deficits.